 Article by:
Article by:
DR. EVAN MALONE
NON-LAWYER
BOARD-CERTIFIED INTERNAL MEDICINE PHYSICIAN
It is not difficult to speak with someone and not have them share their first-hand experience with SARS-CoV-2 infection. If anything, someone close to them has been infected and impacted by the infection.
Rebound and Recovery From Acute Infection
What is not as readily discussed is the rebound and recovery from an acute infection. Acute infection being distinct from a positive test in that there is a period of defining symptoms: fever, myalgia, dyspnea, cough, lethargy, etc.
Just as the spectrum of symptoms is broad – ranging from nuisance, innocent symptoms (loss of smell, mild headache) to the more extreme hypoxia warranting hospitalization – the same is true for the duration of the symptomatic period across various individuals – some limited to less than two days, others spanning many weeks.
Can I Go Back To Working Out/Exercising?
Applying this nebulous symptom severity index and symptom duration timeframe to acute infection in an otherwise active, fitness-minded, perhaps obsessed age-group athlete and leaves one wondering “can I get back to working out?” For the first many months of the global pandemic, this perhaps may have been taken as a bit of a selfish query – the desire to return to exercise when raised in the context of the gravity of the illness for many (death, hospitalization, loss of livelihood).
Along the way, in 2020 we collectively learned about the virus and its impact on the population and the human body. Research into the mechanisms of infection, transmission, prevention, treatment, recovery, and short- and long-term impact – a different study or dataset or conclusion was being published nearly every hour of every day.
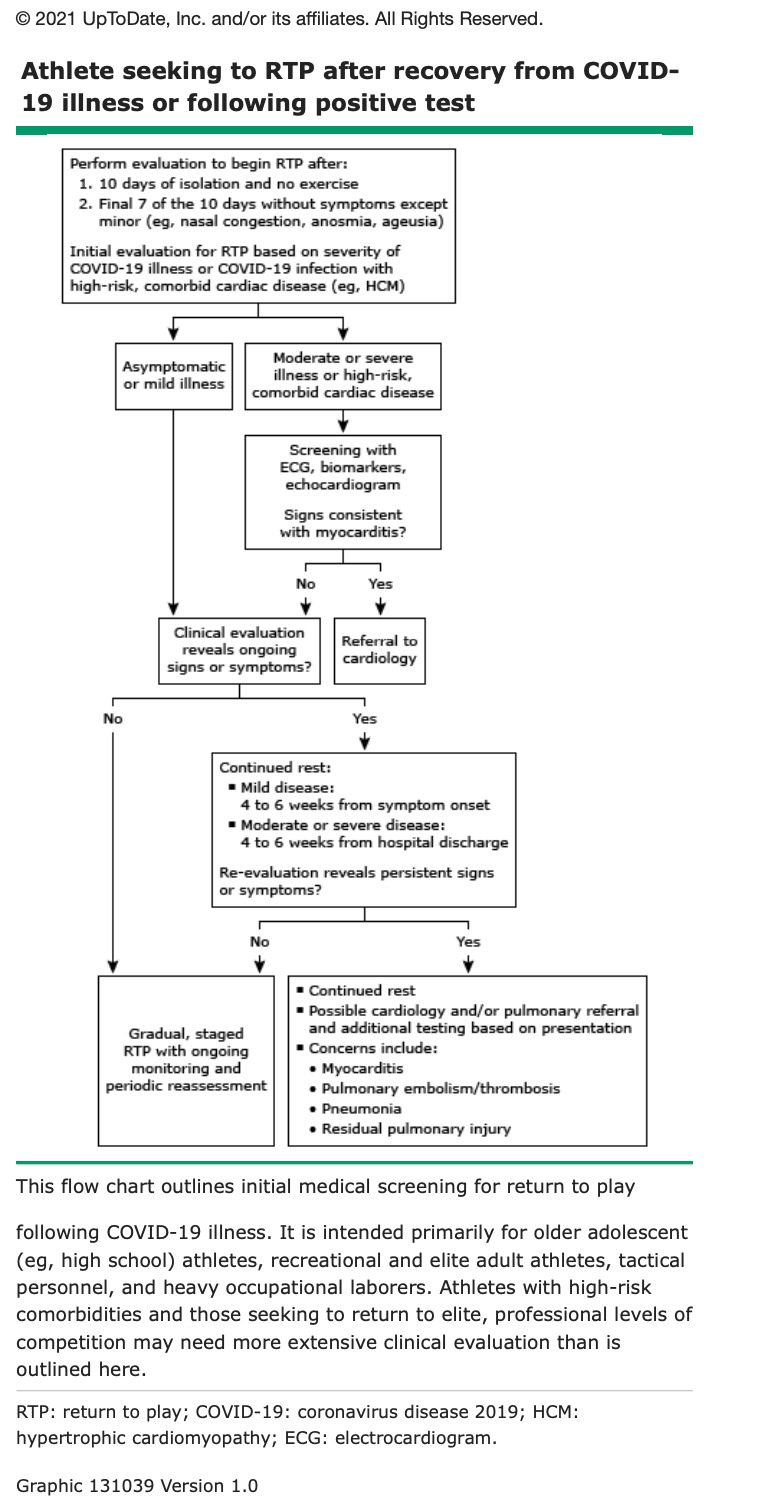
In the late summer of 2020, some guidance began to take shape for the exercise-minded individual recovering from acute infection. Domestically, much of this was driven by research focusing on collegiate-level athletes, to understand when and in what manner it was safe for these young athletes to return to their respective sports.
Joe’s COVID Journey, Recovery, and Return to Exercise.
In Joe’s situation his symptom onset was around September 5, 2020 (Labor Day weekend), his positive PCR sample would result on September 7, 2020. During the next many days his prime goal apart from strict isolation protocol was managing his symptoms and monitoring any systemic manifestations (shortness of breath, chest pain, confusion). As that initial string of days wound by, interrupted by Hurricane Sally (landfall September 15-16, 2020, he would be confronted with fatigue and the sensation of breathlessness which was temporized and stabilized with supplemental oxygen use and a combination of systemic (oral) and inhaled steroid agents. At this point, he understood that this was likely impacting his cardiopulmonary system beyond the simple nuisance symptoms which are mostly contained to the upper respiratory tract (nasal and sinus congestion). This added another layer to what would end up being an additional step to take prior to returning to physical exertion (exercise) which is part of his daily routine as a multi-sport athlete. This was somewhat uncharted territory for both Joe as well as the medical community as a whole – studies were being conducted to best understand the next step or steps to take.
Studies On The Heart and COVID-19 Infection
 One of the first such studies was published on September 11, 2020, in JAMA Cardiology (Rajpal S, Tong MS, Borchers J, et al. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol. 2021;6(1):116–118. doi:10.1001/jamacardio.2020.4916) detailing cardiac evaluation including studies such as the electrocardiogram (EKG), echocardiogram (ultrasound of the heart), and cardiac MRI. The test modality of choice is to be dictated by the severity of the symptoms and the findings along each step of the algorithm. This would provide some guidance as to which athletes were at higher risk for myocarditis, cardiomyopathy, malignant dysrhythmia, or even sudden cardiac death and then to help apply some guidelines on activity limitations moving forward.
One of the first such studies was published on September 11, 2020, in JAMA Cardiology (Rajpal S, Tong MS, Borchers J, et al. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol. 2021;6(1):116–118. doi:10.1001/jamacardio.2020.4916) detailing cardiac evaluation including studies such as the electrocardiogram (EKG), echocardiogram (ultrasound of the heart), and cardiac MRI. The test modality of choice is to be dictated by the severity of the symptoms and the findings along each step of the algorithm. This would provide some guidance as to which athletes were at higher risk for myocarditis, cardiomyopathy, malignant dysrhythmia, or even sudden cardiac death and then to help apply some guidelines on activity limitations moving forward.
Lingering Effect of COVID-19 Infection
So, using that as a launching pad for the discussion with his physician, Joe and his medical provider team decided it was best to proceed with cardiac screening – EKG (electrocardiogram – electrical tracing of the heartbeat and myocardial contraction) and echocardiogram (ultrasound of the heart). These studies would occur in late September, roughly 4 weeks after his initial symptom onset. The tests were not fully “normal” as the echocardiogram (ultrasound image of the heart) revealed some enlargement of the right side of the heart – a potential sign that there was some increased stress or workload on the right side of the heart attempting to pump blood to the lungs for oxygenation (and carbon dioxide removal). This prompted Joe and his medical provider to lean on some of these recent studies and pursue the cardiac MRI study to best visualize and understand if there was any myocardial involvement (i.e. myocarditis) otherwise known as inflammation of the muscle tissue which makes up the heart. Inflamed muscles are something Joe is keenly aware of with his exercise routine, but an inflamed cardiac muscle is not on the same level as inflamed skeletal muscles weary from a long workout or race.
As the cardiac MRI was being coordinated, the instructions were simple: “take it easy and don’t get the heart rate up.” Translated, this meant no exercise. The potential risk being cardiac arrhythmia or heart failure if the already-angry myocardial tissue was additionally stressed.
Fortunately for Joe, the cardiac MRI would reveal normal myocardial tissue and the right side of the heart appeared normal as well. The suggestion of the abnormal right-sided chambers on the echocardiogram was not present (or had resolved with additional time for recovery) on the MRI study.
Joe was now free to get back into his daily exercise routine – only limitation being “do what you can, take it easy getting back into it, and listen to your body.”
WATCH JOE VIDEO ABOUT HIS COVID JOURNEY HERE >
WATCH VIDEO ABOUT DR. EVAN MALONE’S DELTA VARIANT EXPERIENCE >
Fast forward many months later, and very similar guidance has emerged for application to the recreational athlete desiring to return to exercise. The algorithm is meant to accompany the examination by and assessment of a qualified medical professional.
Key Points on Returning To Play.
For any age-group athlete looking to get back to fitness, exercise, physical exertion the first step following the acute infection (i.e. isolation period) should be an evaluation by your primary care provider. A “return to play” or “return to physical exertion” discussion should be had. For some it may be as simple as routine, annual bloodwork, or non-invasive testing. For others it may include a larger, more-involved battery of tests.
Joe Zarzaur is a Board Certified Civil Trial Attorney whose firm is dedicated to promoting community safety since 2007. ZARZAUR LAW’S AREAS OF PRACTICE: Serious Personal Injury, Product Defect, Auto Accidents, Cycling Accidents, Motor Vehicle Accidents, Products Liability, Wrongful Death, Community Safety, Boat and Jet Ski Accidents, Slip and Fall Injuries, and more. Licensed in Alabama and Florida.
If you’ve been the victim of an accident, it’s important that you don’t make any rash decisions. Put yourself in the best possible position to receive the justice you deserve. It is also important to consult with a Board Certified Trial lawyer who has the knowledge and experience to help you. We know accidents can be stressful and want to make the process as easy as possible for you. Call Zarzaur Law, P.A. today at (855) Hire-Joe, or by requesting a free case review through our website.